Precision Oncology
Research Description
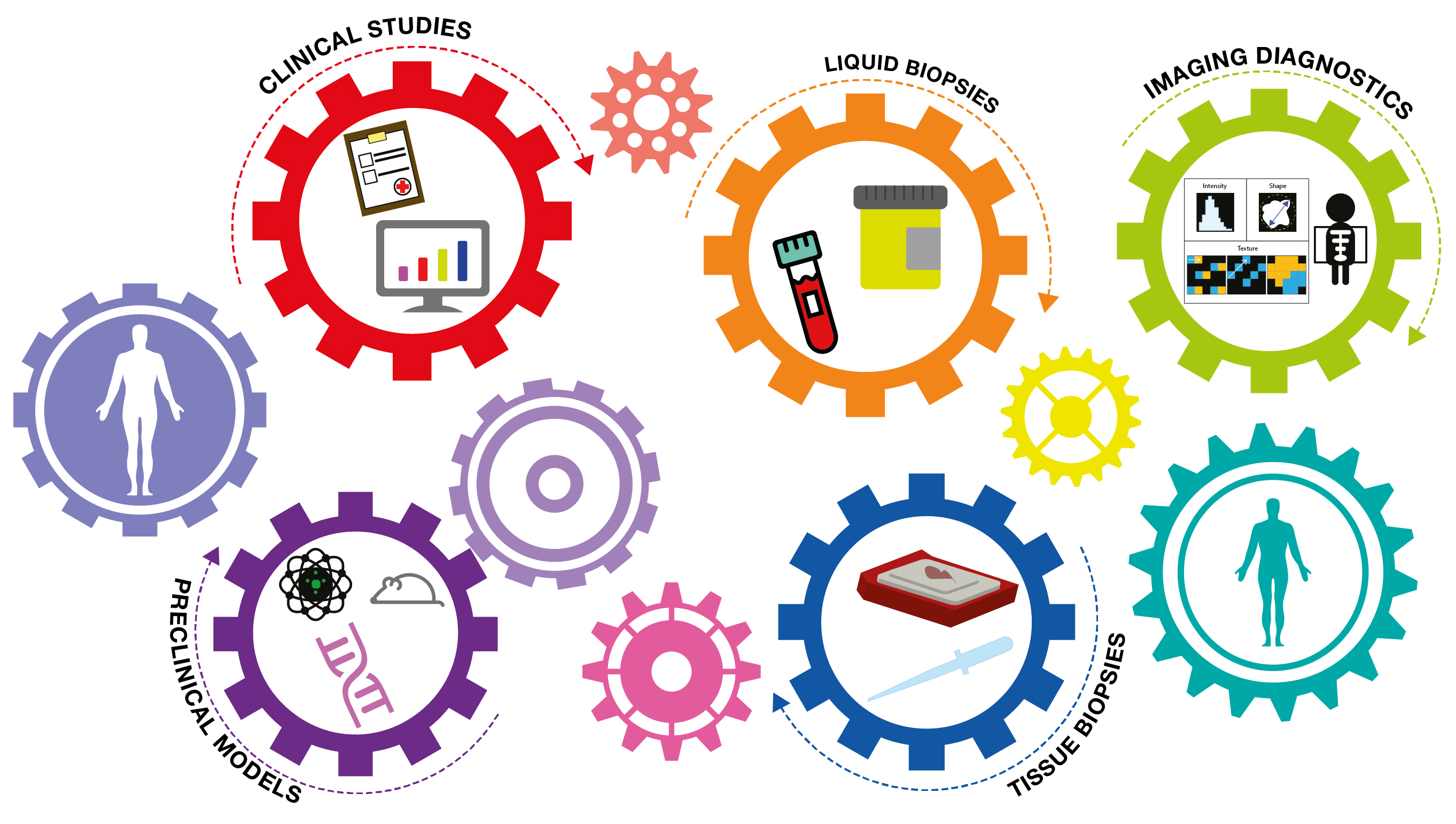
The Precision Oncology Program headed by Silvia Marsoni is the bridge that translates preclinical discoveries into clinical benefit for cancer patients - often referred to the concept From Bench to Bedside. The group has been crucial to sustain the development of two large consortia and clinical networks within the field of colorectal and breast cancer.
Discussion of pre-clinical and clinical evidences with collaborators is essential for the Precision Oncology Unit (POU) to generate hypothesis-driven and "transformative" clinical trials. Thus, POU is focused in trial designing (including protocol and informed consent writing), in supervising study specific-documents, in developing electronic Case Report Forms (eCRFs) and in managing samples shipments and road traffic data produced by our translational partners, acting ultimately as a bridge between clinical centers and laboratories.
Figure 1: CRC and BC networks related to ALFAΩMEGA and METAMECH Master Observational Trials (MOT)
Background
Colorectal cancer (CRC) and Breast cancer (BC) are ranked within the top five lethal cancers. In Italy, the 5-years survival rate for breast cancer is now reported at 87% and falls to the 65% in colorectal cancer. At the beginning of the century these percentages showed a worse scenario, counting 84% and 59% respectively. Although mortality by CRC and BC has progressively declined due to more effective therapies, clinical research has still to satisfy several unmet medical needs such as the post-surgical management of molecular minimal residual disease, how to shift from a "one-type-fits-all" therapy to an individually tailored approach and, last but not least, how to turn hot immunologically cold tumors.
Ongoing Projects
ALFAΩMEGA and METAMECH are two clinical translational platform that will follow a cohort of patients from diagnosis to cure/death to navigate the evolutionary pathways of CRC and BC respectively, during their natural history and under the Darwinian pressure of therapies. These clinical resources for integrative clinical data, imaging and samples collection will allow the molecular story-telling of CRC and BC spread in genetic, functional and immunological terms along time and space, and the selection of appropriate patients for experimentally-driven trials (e.g. PEGASUS in CRC) focused on tumor evolution.
Focusing on CRC, we chose to further investigate within PEGASUS and ARETHUSA trials, two major issues strictly connected with the patients' quality of life.
On one hand, PEGASUS trial aims to establish the feasibility of using longitudinal liquid biopsies (LBs) to guide the post-surgical and post-adjuvant treatments of operable stage III or T4N0 stage II CRC patients. The PEGASUS study couples circulating tumor DNA detection in plasma (LBs) and guided chemotherapy in order to improve patients' clinical outcome and to reduce their toxicity exposure. Importantly, we are addressing the tumor from different research perspectives, thanks to the involvement of PEGASUS patients in the ALFAΩMEGA protocol. This approach allows a comprehensive collection of information that starts from the definition of the single cell molecular pattern and the identification of the tumor immunological landscape, through genome characterization and microbiome analysis. Exploiting artificial intelligence, we are trying to recognize new integrative markers to predict the response to therapies, with the radiologists and pathologists' precious support.
On the other hand, ARETHUSA is an interventional phase II trial in metastatic CRC patients, which attempts to turn mismatch repair proficient (MMRp), "immune-cold" tumors, into hypermutated "immune-hot" tumors by ectopically increasing the mutational burden in cancer cells with a DNA-alkylating agent that can drive inactivation of the MMR machinery. Patients with immunologically hot-induced MMRp tumors or with MMRd/MSI tumors, which are more likely to achieve a clinical response from immunotherapy, are then treated with a PD-1 inhibitor.
In BC, up-and-coming experimental results are currently being considered to finalize the design of a study for a treatment that could restore the immunocompetent system of so-called triple negative tumors - with a particularly bad prognosis.